Age Related Macular Degeneration Introduction
Age-related Macular Degeneration (ARMD) is the leading cause of legal blindness in patients over the age of 50, with about 1 in 7 Australians in this age group displaying some signs of the disease. The macula is the very small area at the centre of the retina, which is the film in the camera in the back of the eye that lets you see. The macula is responsible for our fine and detailed central vision necessary for tasks such as reading, driving and recognising faces. As the name suggests, ARMD is a degenerative condition which can result in loss of the central vision. The peripheral vision is almost always preserved.
Types of ARMD
ARMD can be divided into ‘Dry ARMD’ and ‘Wet ARMD’, but they are really an extension of the same problem. The retina is very metabolically active, which is to say that it uses a lot of oxygen and nutrients in order to function, and this creates a lot of waste products. In young healthy eyes, these waste products are removed by the layer underneath the retina called the ‘retinal pigment epithelium’ (or RPE). But in eyes with macular degeneration, the RPE starts to malfunction and waste products accumulate into lumps we call ‘drusen’. Some patients tolerate these drusen without any problems, but in other patients, the immune system starts to attack them and this drives in blood vessels that can leak and bleed. The fluid leaking from these blood vessels is what defines ‘Wet’ ARMD.
- Dry (Atrophic) Macular Degeneration
- This is by far the most common form, accounting for approximately 90% of macular degeneration diagnoses. Dry ARMD generally progresses very slowly as drusen build up under the macula. Vision tends to decline only in advanced stages when large areas of retinal cells are lost at the macula, leaving areas of wear and tear that look like worn carpet. We call this ‘geographic atrophy’ because the patches of wear and tear resemble islands on a map
- Regular eye exams and self-monitoring with an ‘Amsler grid’ are recommended to ensure any changes are picked up early as some patients with Dry ARMD can develop Wet ARMD which requires prompt treatment
- Wet (Neovascular/Exudative) Macular Degeneration
- Though much less common, Wet ARMD can be much more devastating and is responsible for over 90% of cases with significant vision loss in ARMD patients.
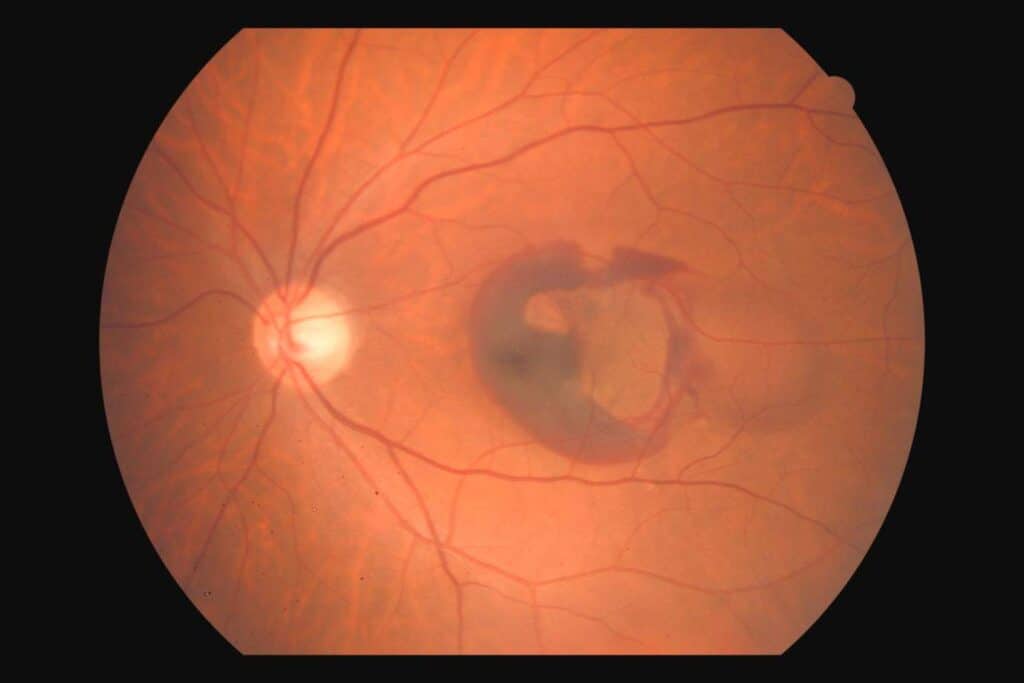
- Wet ARMD is an advanced form of macular degeneration where new and abnormal blood vessels grow beneath the retina. These abnormal vessels leak and bleed into or under the macula, often causing rapid and devastating central vision loss
- With early detection, revolutionary treatments are available which have been shown to preserve vision in the majority of patients
Risk Factors (characteristics that increase the risk of ARMD)
- Age – the risk of ARMD rises steeply with advancing age
- Smoking – smokers are not only 2-4 times more likely to develop ARMD but are also more likely to develop it at a younger age. Smoking is the most important modifiable risk factor, meaning that the most important thing you can do to reduce your risk if you are a smoker is to quit!
- Family history or genetic susceptibility is a strong risk factor with family members shown to have a three times higher risk of developing the disease. Several genes have shown association with ARMD and are currently the subject of intense research.
- Sex – females are at higher risk of developing ARMD than males
- Race – Caucasians are at greatest risk of ARMD, however Asians are more likely to have a specific variant of ARMD called Polypoidal Choroidal Vasculopathy (PCV)
- Obesity and cardiovascular disease also increase the risk of ARMD
What are the symptoms?
The vast majority of macular degeneration patients will experience minimal visual symptoms during the early stages of disease. For most people ARMD does not impair their vision, however it is important to maintain regular checks by the optometrist (in the early stages) or ophthalmologist (in the later stages) to identify any subtle changes or progression and ensure treatment is started in a timely manner.
Symptoms which you may notice include:
- Blurred vision and difficulty focusing or reading
- Difficulty recognising or distinguishing faces
- Distortion (straight lines can appear wavy or objects can appear bigger or smaller)
- Dark patches in your central vision
- Sudden and significant drop in vision
How is it Diagnosed?
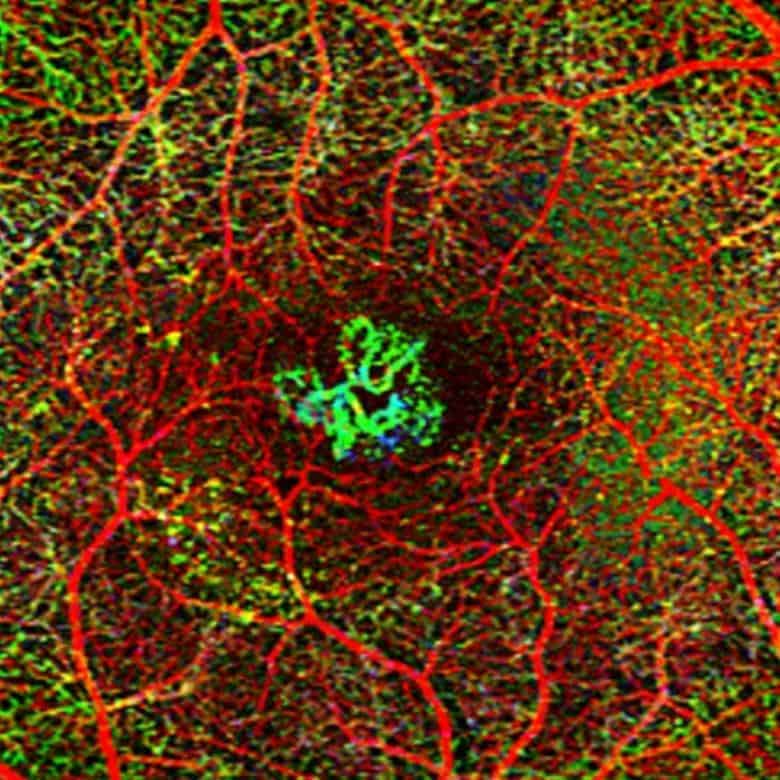
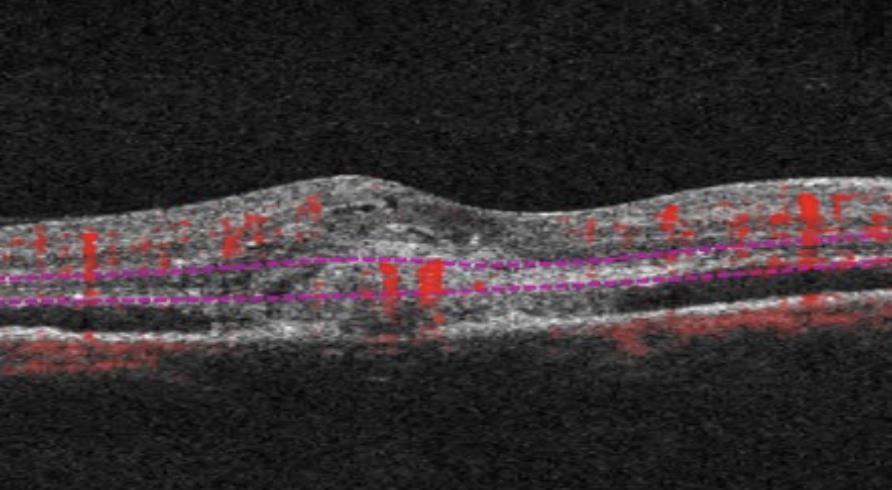
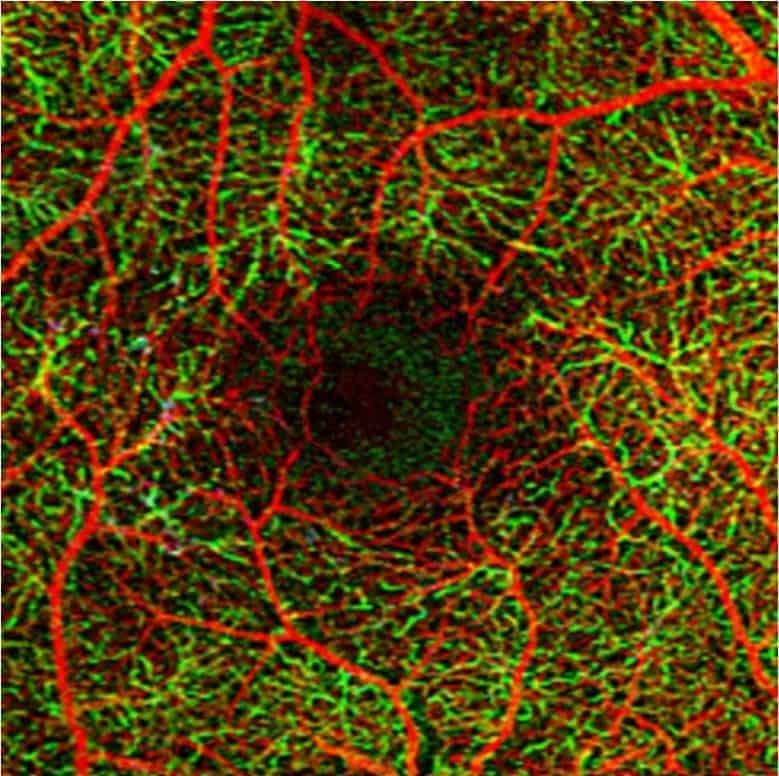
Your pupils will be dilated in order to thoroughly assess the retina. Investigations may be performed including photography, OCT (laser scans), OCTA (a laser-guided assessment of the blood supply), or fluorescein angiography (a photographic test with a special dye). These tests help the doctor assess the severity, check for progression of disease, and monitor response to treatment.
Treatment
- Observation and Lifestyle Changes – in early and intermediate stages of ARMD where vision is preserved, close observation and lifestyle changes are typically all that is necessary. Use of vitamin supplementation and the Amsler Grid for self-monitoring, as well as lifestyle modifications such as dietary changes, smoking cessation, and weight loss are often advised.
- Intravitreal Injections of ‘anti-VEGF’ medications such as Lucentis, Eylea or Beovu are used if there is evidence of Wet ARMD on examination or imaging. These injections can be very effective in reducing the leakage from the abnormal blood vessels, thereby drying out the macula and improving the vision. They can also prevent the continued growth of the underlying blood vessels. The injections are performed with a very fine needle and local anaesthesia to make the eye numb and are usually very well tolerated. These revolutionary medicines have become the mainstay of treatment for Wet ARMD and offer patients unprecedented visual gains and stability, particularly if disease is detected early. Monthly injections are typically required initially, with the interval extended over time. Unfortunately, the vast majority of patients will experience recurrence of disease if treatment is ceased, and hence long-term treatment is typically required.
What Can You Do?
There are several modifications that patients with ARMD (or at risk of it) are able to implement to help reduce the risk of progression. These include:
- Nutrition – Several large population studies have demonstrated that nutrition plays a role in optimising macular health and reducing the risk of macular degeneration. A healthy, well-balanced diet is good for overall wellbeing as well as eye health.
- Lutein and Zeaxanthin are two important pigments found in high concentrations in a healthy macula. Dark green leafy vegetables such as kale, spinach and broccoli are rich in Lutein whereas coloured vegetables such as corn and yellow capsicum as well as egg yolks are rich in Zeaxanthin.
- Omega 3 fatty acids may also prevent damage to the retina with studies indicating that people with a high concentration of these fatty acids in their diet are less likely to develop ARMD. Cold water oily fish such as salmon, tuna and mackerel as well as plant-based flaxseed, walnuts, and chia seeds are good sources.
- Vitamin supplements – The US National Eye Institute’s series of Age Related Eye Disease Studies 1 & 2 (‘AREDS’ 1 & 2) demonstrated that high doses of certain vitamins and antioxidants modestly delayed or prevented progression of intermediate to advanced disease. While there are many vitamin supplements marketed for ARMD, it is important to find the correct vitamins and concentrations that have been proven effective. The AREDS 2 formulation consists of Vitamin C 500mg, Vitamin E400 IU, Lutein 10mg, Zeaxanthin 2mg, and Zinc 8mg.
- Smoking cessation– reduces the risk of development and progression of macular degeneration as well as improve overall health
- Self-monitoring with an Amsler grid– weekly testing of each eye using the Amsler grid looking for any new changes to the vision is an important tool in identifying changes early. Amsler Grids along with directions for use can be provided by your doctor or found on the internet
- Attend regular eye checks – early detection is key to success
Key Points
Though macular degeneration is a leading cause of blindness, it is important to recognise that only central vision is typically affected and total blindness is rare. Patients with end-stage disease are still generally able to navigate well indoors and outdoors however they will have difficulty with high acuity tasks such as reading and driving. Regular eye exams are essential for detecting macular degeneration early to slow its progression and minimise the chance of permanent vision loss. Modern treatments have revolutionised the outlook for patients with this condition, but are typically required long-term. Living a healthy lifestyle by eating well, exercising regularly, and avoiding smoking can help reduce your risk of developing macular degeneration and slow its progression.

Contact us to get help with any questions you may have, or support you may need.

