Retinal Vein Occlusions Introduction
The retina is the photographic film in the camera in the back of the eye that lets you see. Retinal vein occlusion (RVO) occurs when one of the veins draining blood from the retina becomes blocked. This causes varying degrees of vision loss depending on the location, severity and number of blood vessels involved. It is the second most common cause of blindness from retinal vascular disease after diabetic retinopathy.
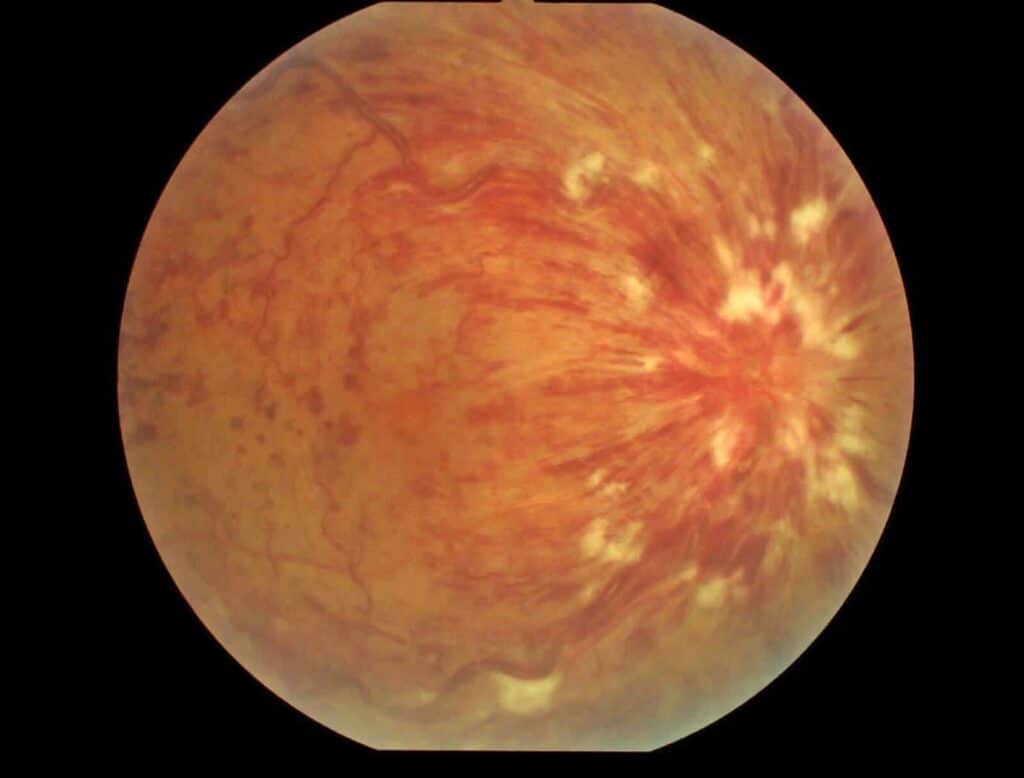
Arteries deliver blood throughout the body and veins drain it away. When the veins become blocked, it is a bit like stopping a creek from flowing – pressure builds up and the fluid ‘breaks the banks’ causing retinal haemorrhages (bleeding) and retinal swelling. The reduced blood flow through the eye starves the retina of oxygen and nutrients, causing some degree of damage. The retina is like a delicate electrical circuit and it doesn’t mix with fluid very well – hence vision is reduced, patchy, and sometimes distorted when it is swollen.
Types of RVOs
RVOs are classified according to the location of the blockage which directly influences their presentation, management and prognosis.
- Central Retinal Vein Occlusion (CRVO) – occurs when the main vein is blocked. These usually have the poorest prognosis.
- Hemi-Retinal Vein Occlusion (HRVO) – occurs when the whole top or bottom half of the retina is affected by the blockage.
- Branch Retinal Vein Occlusion (BRVO) – occurs when one of the smaller veins is blocked, affecting just a patch of the retina.
Risk factors
RVOs are more common with:
- Advancing age
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Being overweight
Less frequent associations include blood disorders, inflammatory conditions, and high pressure in the eye.
What are the Symptoms?
Symptoms can vary depending on the type and severity of RVO. Generally, RVOs cause a sudden, painless drop in central or peripheral vision. Less commonly, patients can complain of floaters or a sudden loss of all vision if the initial blockage went unnoticed and more serious complications have developed.
Visual loss can occur through 3 mechanisms:
- Swelling of the macula (ie. the central part of the retina that serves your fine central vision), termed ‘Cystoid Macular Oedema’
- This is the most common cause of visual loss from RVO and occurs due to leakage of the vessels upstream from the blockage which results in swelling of the macula.
- Ischaemia
- In severe blockages, there is no blood flow and the lack of oxygen results in areas of irreversibly damaged retina
- Neovascularisation
- The body’s natural response to poor blood supply is to grow new blood vessels (termed ‘neovascularisation’). Unfortunately, these new vessels grow like weeds in the eye and are fragile and can leak and bleed. Left untreated, these abnormal blood vessels can cause problems such as extensive bleeding (‘haemorrhage’), a nasty form of glaucoma, and complicated retinal detachment that can be very difficult to manage.
How is it Diagnosed?
Your eyes will be thoroughly assessed after dilating your pupils. Investigations may be required including OCT scans, retinal photography, and fluorescein angiography (a photographic test with special dye). These tests help the doctor assess the severity as well as monitor progression of disease and response to therapy.
Treatment
- Observation – in mild cases where vision is preserved, close observation may be all that is necessary
- Intravitreal Injections of ‘anti-VEGF’ medications such as Lucentis, Eylea, Beovu; or steroid medications such as triamcinolone or Ozurdex – if the vision is reduced due to swelling of the macula, intravitreal injections can be very effective in reducing the swelling and improving the vision. They can also prevent the growth of new blood vessels described above (neovascularisation). The injections are performed with a very fine needle and local anaesthesia to make the eye numb and are usually very well tolerated. These revolutionary treatments have been a minor miracle in terms of the outlook for patients with these (and other) retinal conditions, and can effectively reduce the swelling, reduce the risk of further deterioration, and often result in significantly improved vision, particularly if disease is detected early. Monthly injections are typically required initially, with the interval extended over time, and potentially ceasing after a couple of years in many RVO patients.
- Laser – in severe cases where abnormal blood vessels develop (neovascularisation), laser treatment is used to destroy the damaged retina which is driving their growth. This is done to reduce the risk of developing a painful blind eye.
- Surgery – vitrectomy surgery is occasionally required when the abnormal blood vessels cause extensive bleeding or scar tissue formation.
What Else Can Be Done?
- Management of cardiovascular risk factors – good control of blood pressure, blood sugar levels (in diabetics), cholesterol, and weight as well as cessation of smoking will reduce the risk of further blockages in the other parts of the body including the other eye, brain, and heart
- It is very important to maintain regular eye checks following RVOs as severe complications may develop insidiously, possibly leading to a blind painful eye
Regular eye reviews are key to detecting progression and allowing prompt treatment where necessary.


Helpful links: Epiretinal Membrane, Macular hole, Central Serous Chorioretinopathy, Allergic Eye Disease, Keratoconus

